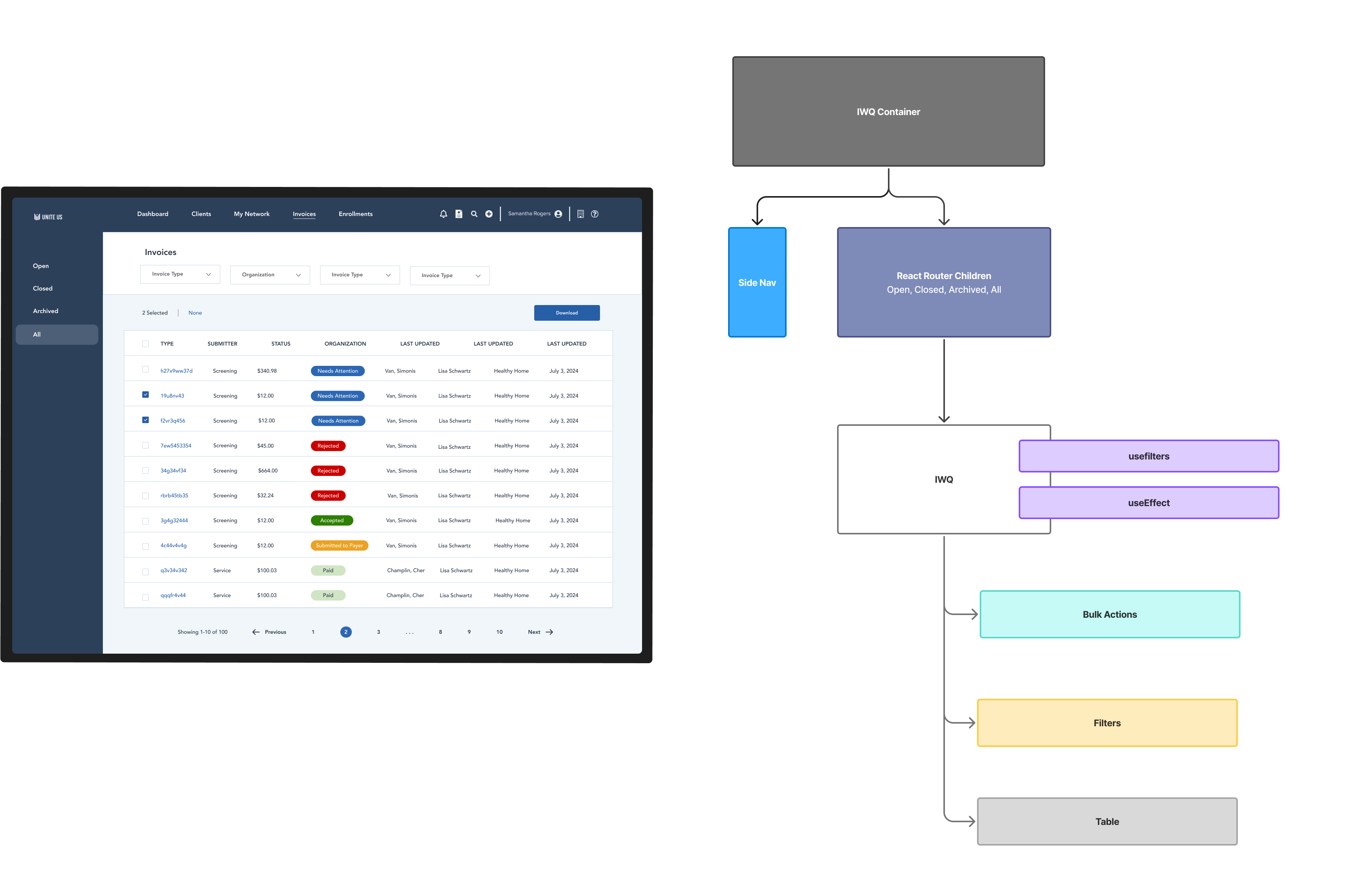
Payer Invoice Work Queue
The Payer Invoice Work Queue is a table that allows Payers in social care to track invoices submitted by Community Based Organizations (CBOs) for the reimbursement of services they provided (food, housing, transportation, etc). I led the technical design for this initiative, and the UX design for its enhancements to workflow efficiency.
ROLE
Design Engineer
IMPACT
Facilitated reimbursement of $152M+ to Community Based Organizations (CBOs) in North Carolina and reduced payer invoice rejection rate from the national average of 18% to 1.5%
Challenge
Users expressed that they are often duplicating the same task for hundreds of similar invoices. We needed a way to group invoices, and take bulk actions on all of them at the same time. The table design also wasn't intuitive to users. The filters were too far away from the table, and the bulk download button wasn't properly grouped with the other filters.
Approach
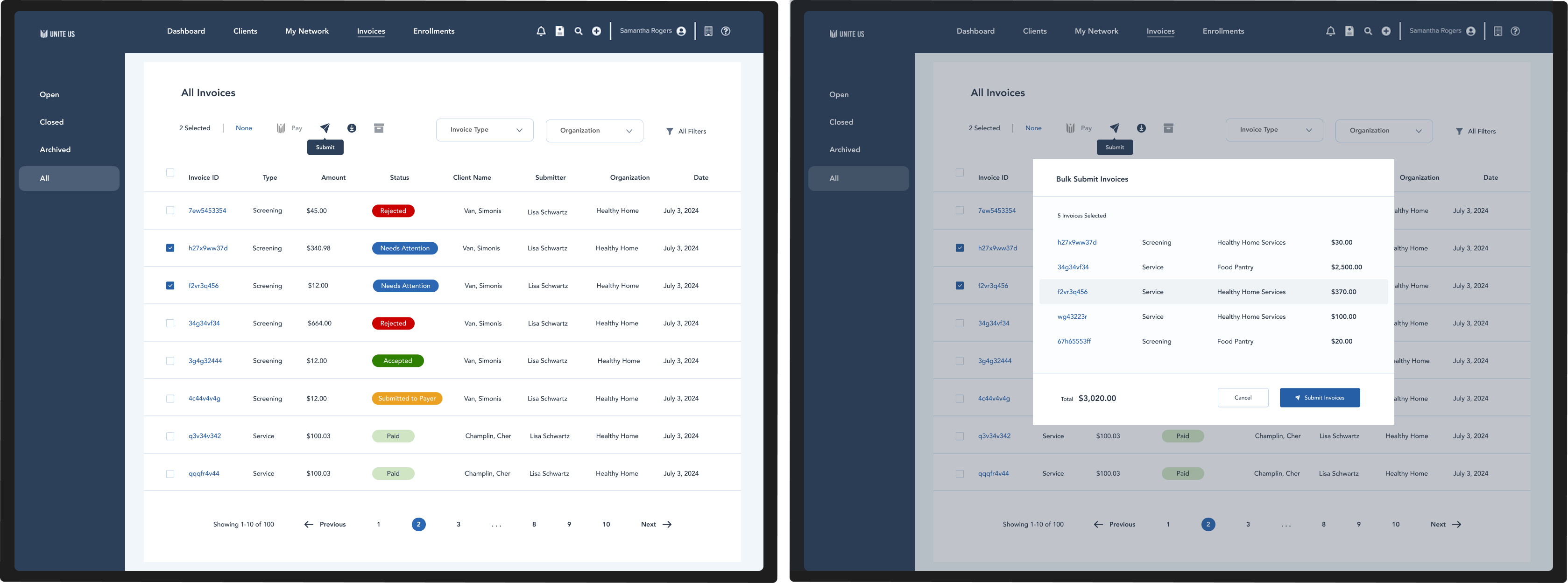
Bulk Actions
Users have had to go through hundreds of invoices one at a time, greatly reducing their efficiency. I designed bulk actions to the Payer Work Queue which allows users to group related invoices and respond to them at the same time.

User Assignment
Users have said that it can be difficult keeping track of when an invoice is already being looked at by a colleague. I designed the ability to assign invoices to users, and give them "In Review" statuses.