NY Medicaid 1115 Waiver
The NY 1115 Medicaid Waiver is an investment of over $7 billion through 2027 in expanding Medicaid into innovative solutions for holistic, value based care addressing systemic needs like food insecurity and housing stability. Unite Us was selected to serve as the infrastructure for this initiative.
I led the designs of an eligibility assessment, screenings to identify the client's social care needs and determine their eligibility for the Waiver program. The challenge was in simplifying a complex workflow involving diverse user roles including CBOs, healthcare providers, and MCOs. To solve this I designed a care plan that combines our disjointed feature sets.
ROLE
Lead UX Designer
IMPACT
Connected the CBOs, healthcare providers, and MCOs in 9 of the 13 New York State regions, representing 72% of Medicaid members across the state.
Challenge
%202.png)
The NY Waiver has a diverse set of user and client types that have different needs throughout the workflow. I started this work by laying out the workflow end-to-end, blue squares representing client entry points and purple squares representing users (case managers and SCN Leads).
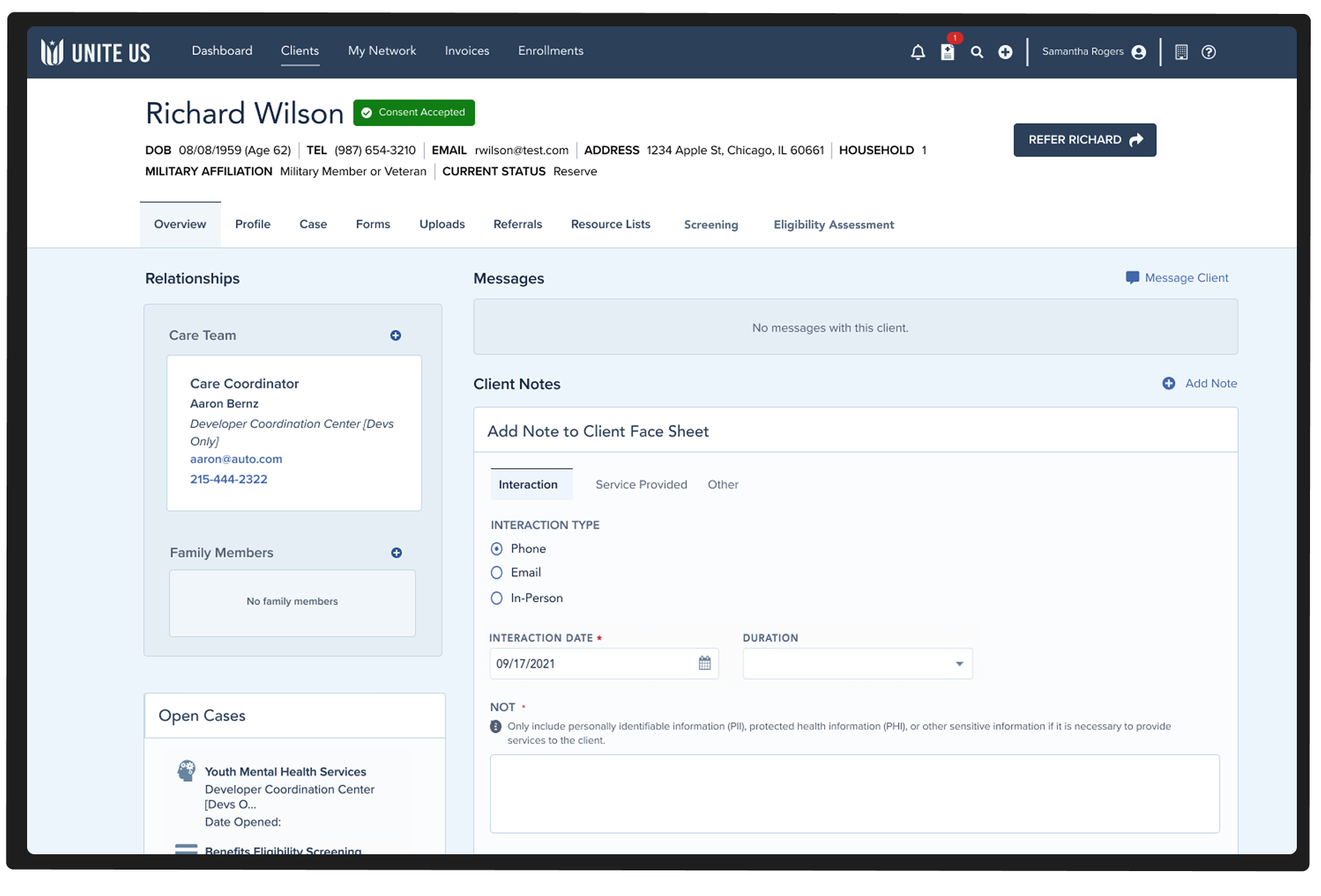
The features of our platform are inherently disjointed. This is the client's facesheet - it gives no clear indication of where the client is in their care journey, making it difficult for care managers to identify the next best action.
Approach
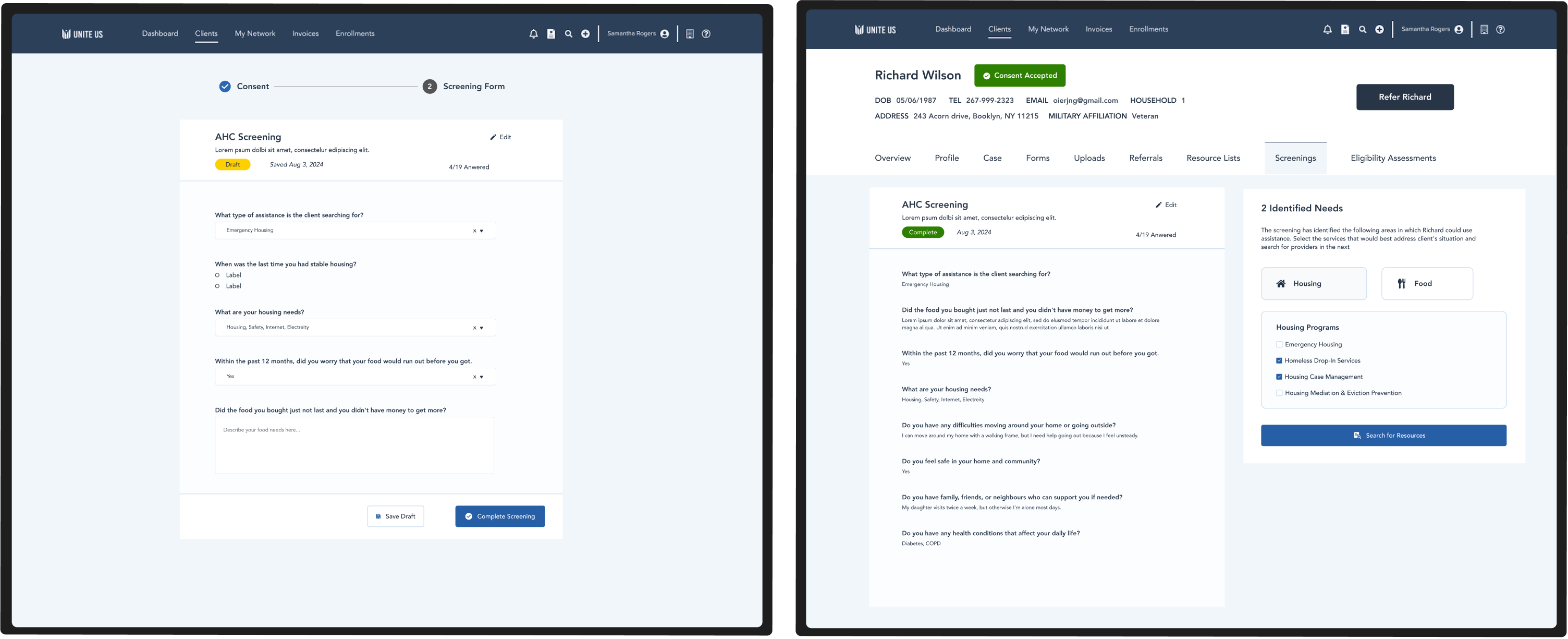
Screenings
The first step of a client's journey is to identify social needs. I designed a way to categorize these needs in a simple way, so that the care manager can easily refer the client to the correct programs.
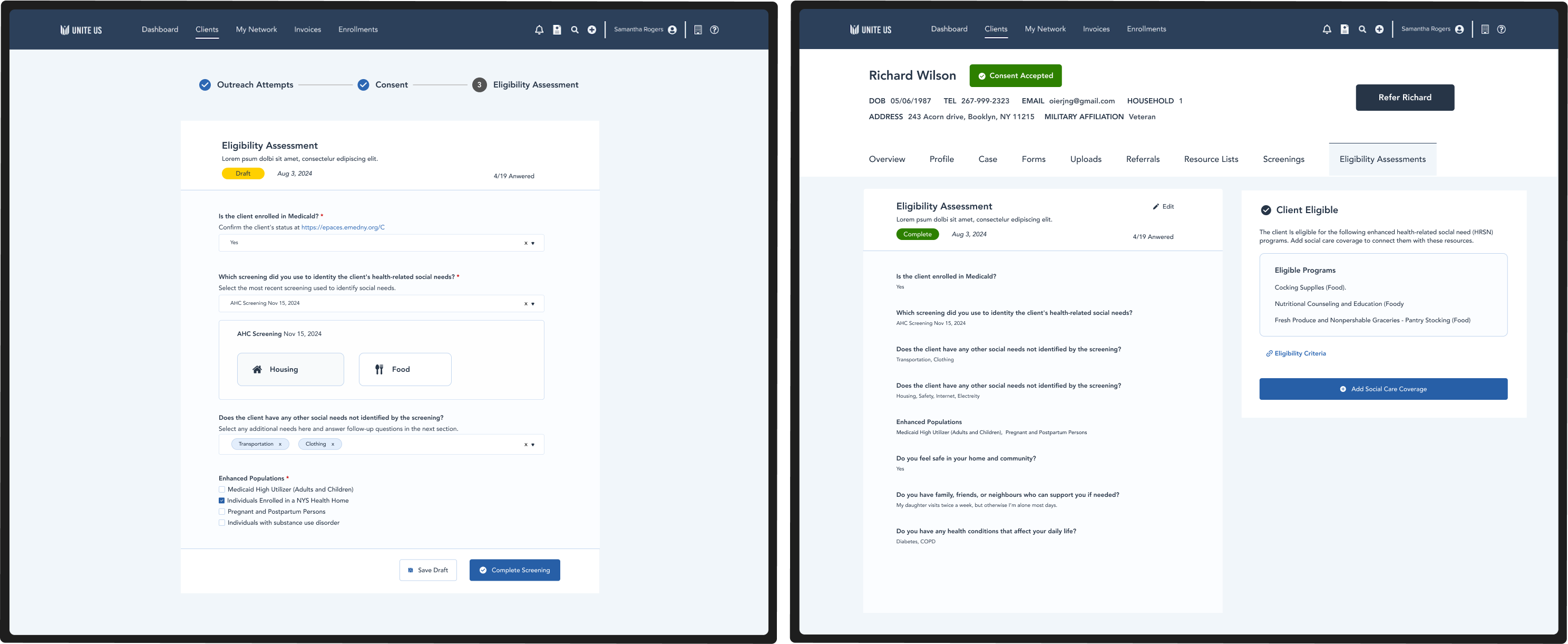
Eligibility Assessments
Users need to determine whether the client is eligible for "paid programs" where CBOs can be reimbursed for providing services. We designed a form that dynamically asks questions based on the client's unique needs.
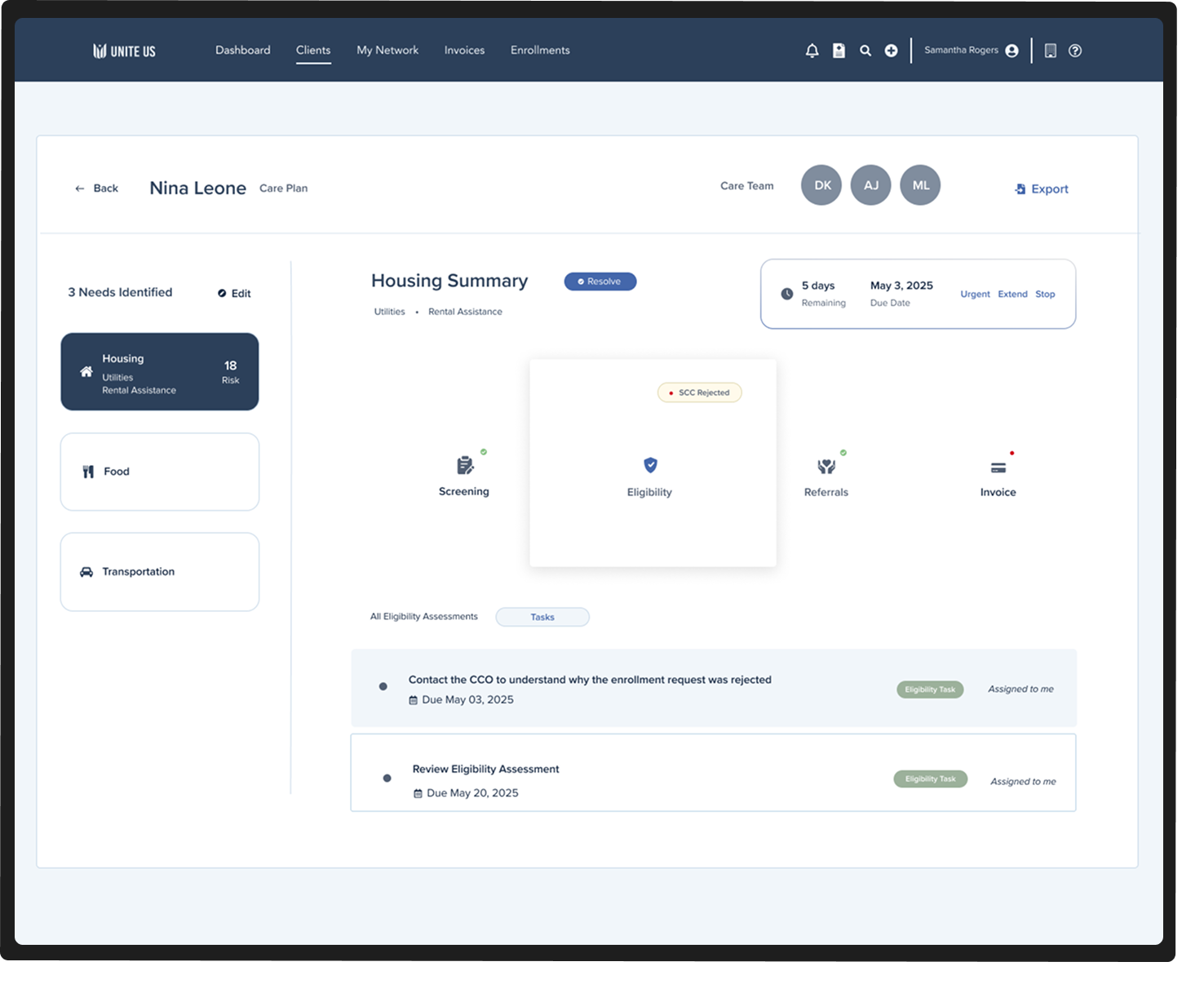
Care Summary
This care plan summarizes the clients care journey. It is an interactive map, allowing users to jump in and out of workflows for a specified need. This solved the problem of an overly complex platform with disjointed feature sets.